New research presented Wednesday at the Alzheimer’s Association International Conference in Amsterdam highlights a growing body of evidence linking people’s microbiomes to their brain health.
One study found that chronic constipation was tied to worse cognitive abilities — the equivalent of three years of aging — while two other studies found that certain gut bacteria were associated with dementia risk.
All three studies, which haven’t yet been published in peer-reviewed journals, point to a possible role that a buildup of “bad” bacteria in the gut could play in cognitive health.
“We know that it is essential for overall good health to regularly eliminate waste from the body. If that does not happen, we may retain toxins that negatively impact our health in a variety of ways,” said Christopher Weber, the director of global science initiatives with the Alzheimer’s Association, who wasn’t involved with the research. “Although more research is needed, it’s a fascinating start.”
When ‘bad’ bacteria overcrowd the ‘good’
Chaoran Ma, an assistant professor of nutrition at the University of Massachusetts Amherst, led the study looking at constipation and cognitive decline, which analyzed data on bowel movements and cognition over six years from 110,000 people from three long-running studies.
People with chronic constipation — defined as having one bowel movement every three or more days — were found to have “significantly” worse cognition, equal to three years of aging, compared to those who were able to go once a day, the research found.
People with chronic constipation also had more bacteria that cause inflammation in their guts and less bacteria that break down dietary fibers, said Ma, who was a research fellow at Brigham and Women’s Hospital and Harvard Medical School in Boston when the research was completed. The research showed a correlation, not causation, meaning the study doesn’t prove constipation causes such problems.
Researchers don’t know why constipation may affect the brain that way, but they speculate that a buildup of “bad” bacteria overcrowds the “good” protective kind, Weber said.
Ma said the findings are particularly important for older adults, who are more likely to experience constipation due to lack of exercise, use of certain medications and fiber-deficient diets.
Two other studies presented at the conference, both of which were conducted by researchers at UT Health San Antonio in Texas, found that specific gut bacteria were associated with an increased risk of dementia in cognitively healthy adults. Other gut bacteria, they found, had protective effects.
Together, the findings join a growing body of data about what scientists call the gut-brain axis — the two-way communication pathway that connects the functions of the gastrointestinal tract and the brain via the nervous, immune and hormonal systems and is involved in a variety of processes, from metabolism to stress.
A better understanding of the axis could help scientists develop new ways to prevent and treat Alzheimer’s and other dementias even before symptoms emerge.
“It is important to recognize that all of our body systems are connected and work together,” Weber said. “If one of them isn’t working well and it is not properly diagnosed and treated, it can have significant consequences for the health of other areas of the body.”
A dementia biomarker in the gut?
Past research has found that people diagnosed with Alzheimer’s disease, as well as obesity, diabetes, irritable bowel syndrome and Parkinson’s, have less diverse gut microbiomes compared to those without the disease.
A study conducted in Japan and published last year in the journal CNS Neuroscience & Therapeutics found that Alzheimer’s patients with constipation experienced cognitive decline two times faster than patients without constipation.
However, less is known about how — and whether — doctors will one day be able to use such gut changes to reliably spot dementia in people who still have healthy brains or treat it in those who already have symptoms.
“Each person seems to have a unique microbiome, almost like a fingerprint,” said Dr. Monia Werlang, a gastroenterologist and clinical assistant professor at the University of South Carolina Greenville Medical School. “Scientists are still learning how to manipulate it to promote health and to modify disease. Targeting the microbiome is promising, but there are many unknowns, especially considering the variability from person to person.”
Perhaps the biggest unknown is whether Alzheimer’s causes bacterial changes in the gut or whether bacterial changes in the gut, brought on by constipation, for example, cause Alzheimer’s, said Rima Kaddurah-Daouk, a co-principal investigator with the Alzheimer Gut Microbiome Project, a collaborative research initiative that is mapping the gut-brain axis and exploring how diet and other lifestyle interventions influence cognition.
Zooming in even more, are the bacteria themselves toxic to the brain, or are certain byproducts of the bacteria to blame?
“The bacteria that live with us are our partners, for better or worse. Together we are completing each other’s metabolism and producing a host of chemicals,” said Kaddurah-Daouk, who’s also a psychiatry and behavioral sciences professor at the Duke University School of Medicine in North Carolina. “The new research is a good first step, but we have to get to the molecular level and connect the dots.”
For example, a reduction in one type of bacterial byproduct, called butyrate, as detected in Ma’s study may partly explain why constipation is associated with poorer cognition.
Butyrate is produced in the gut when certain bacteria break down dietary fibers. It interacts with the immune system and helps reduce inflammation in the brain and the spinal cord, Ma said. Butyrate also protects the blood-brain barrier, helping it better prevent toxic molecules from entering the brain.
When fewer of the butyrate-producing bacteria exist, the brain becomes more vulnerable to “bad” molecules that invade it and could worsen cognition. The natural aging process also favors an increase in inflammation-causing bacteria, which can lead to a “leaky gut,” further allowing toxic chemicals to travel into the brain, according to research published last year in the journal Nutrients.
Although a “healthy” gut microbiome hasn’t been defined yet, there’s plenty of evidence that shows balance is key. In fact, an imbalance in the gut, known as dysbiosis, has been associated with the development of anxiety, obesity, diabetes, depression, multiple sclerosis, chronic fatigue syndrome and other disorders, the same paper said.
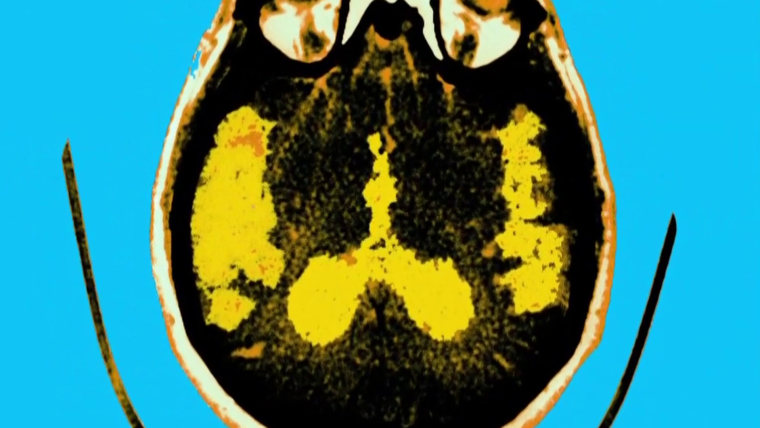
More work is needed before experts can use the gut microbiome as a screening tool for Alzheimer’s and other dementias, which would be less invasive and more convenient than the brain scans or spinal taps currently used to diagnose the disease.
Dr. Shae Datta, a neurologist and co-director of the NYU Langone Concussion Center, said having a biomarker like gut bacteria could “provide a window into dementia that could perhaps help us start patients on medications and preventive means of lifestyle modifications earlier on,” which is critical to treating Alzheimer’s.
Studies consistently show that exercise, sufficient sleep and a proper diet consisting of fiber-rich foods (particularly a Mediterranean diet) will not only prevent constipation, but also promote brain health.
“It’s time to stop seeing Alzheimer’s as just a disease of the brain, but rather as a disease of the brain, liver and gut,” Kaddurah-Daouk said. “Changing your lifestyle for the better — eating right, exercising, alleviating stress — is more effective than any pill available for Alzheimer’s today.”
Follow NBC HEALTH on Twitter & Facebook.